Normal v. Common: Women’s Pain
Get any group of women together and the conversation will, at some point, turn to shared pain. How much did it hurt when you had your IUD inserted? Have you physically recovered from childbirth? What works for your menstrual cramps? And, most frequent of all: is what I’m feeling normal?
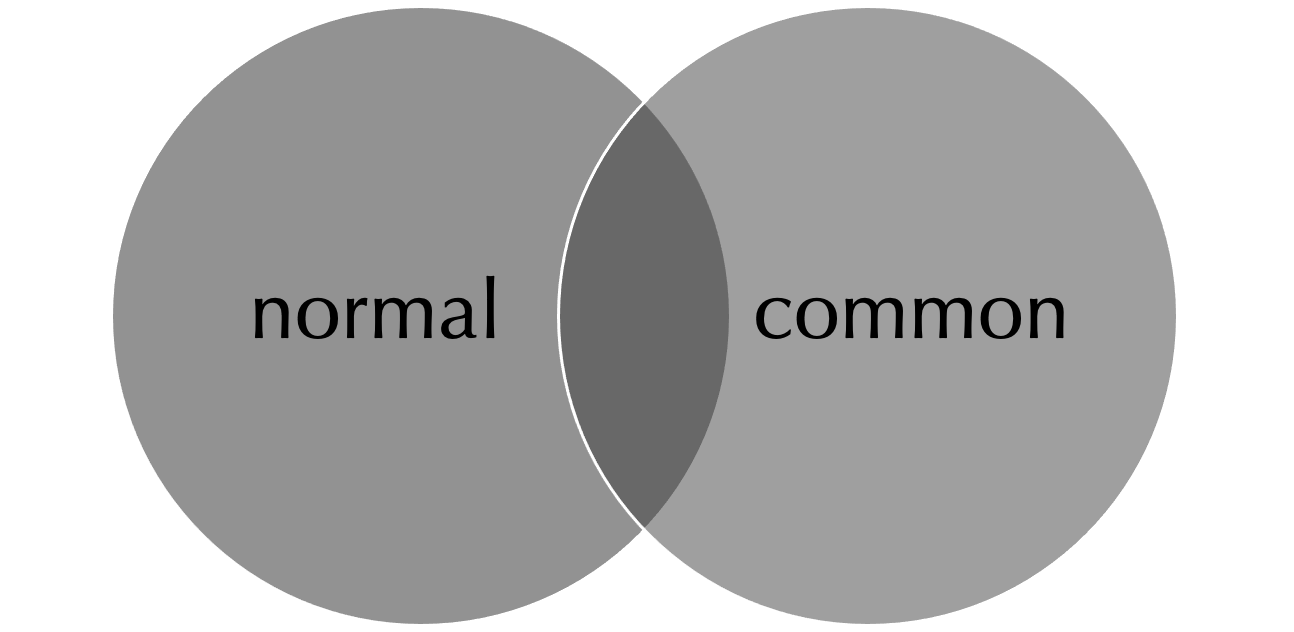
One thing I’ve realized over the last year or so is how wide the gulf is between what’s normal and what’s common when it comes to women’s pain. No, that’s not the right visual; it’s more of a Venn diagram.
In my purely lay and anecdotal experience, we assume our pain is normal because it is so common - and because women’s pain is so often dismissed by doctors, we often assume that both “common” and “normal” equate, from a medical perspective, to “not cause for undue concern.”
A 2002 literature review in the AMA’s Journal of Ethics confirms this, writing that “women are more likely than men to be undertreated or inappropriately diagnosed and treated for their pain.”
“Women's pain complaints are often written off as emotional responses, which explains the finding that women are prescribed psychotropics more often in pain treatment whereas men are given analgesics.”
A 2022 Washington Post piece highlights the pervasiveness of this especially in regards to issues surrounding the reproductive system and reproductive health. Citing a journalist with first-hand experience: “‘There’s a pain gap, but there’s also a credibility gap,’ said Hossain, author of The Pain Gap: How Sexism and Racism in Healthcare Kill Women. ‘Women are not believed about their bodies — period.’”
There are so many complicated reasons for this - okay, really, there’s one and it’s pretty simple: sexism - that you can read about in academic literature (like “The Girl Who Cried Pain: A Bias Against Women in the Treatment” and the follow-up, written two decades later, cleverly titled “The Woman Who Cried Pain: Do Sex-Based Disparities Still Exist in the Experience and Treatment of Pain?”) but the end result is that we’re in more pain for longer than we should be.
My own recent example of this and the reason I’m writing this post is a bad case of sponsylolisthesis which took me almost six years to resolve but that was, in the end, vanquished. I wish I’d taken my pain more seriously and to start, sought treatment sooner; once I did, I wish I had pushed harder for a long-term solution.
I began experiencing debilitating sciatica in my right leg in early 2018, soon after my first child was born. I remember having to excuse myself from donor events after I returned to work from maternity leave, crying with pain in the bathroom as I tried to contort my back and legs into positions that would provide even a little relief. I assumed that whatever caused the pain was a residual effect of pregnancy and childbirth; after all, your body changes so much when you carry and bear a child. And isn’t pain just the price you pay for having a baby? Even pain that lingers long after your newborn has become an infant and then a toddler?
It wasn’t until 2019 that I finally went to a doctor about the pain. My original orthopedist took x-rays and did an MRI and diagnosed spondylolisthesis, the displacement of a vertebra in which the bone slides out of its proper position onto the bone below it. My L5 vertebra had slipped forward enough that it was pushing on my sciatic nerve, and he prescribed a PT regimen to help alleviate the pressure and pain. He was a lovely man - he’d cast my broken bones when I was a child - and I knew he tended cautious in his treatment but, even after months of PT, it never occurred to me to ask if there were other, more intense interventions we could try.
Over the next three years, the pain came and went, fluctuating between a 4 and an 8 on my internal pain scale for months at a time. I kept trying new bouts of PT and occasional appointments with a chiropractor, who used a TENS machine that provided short-term relief. Interestingly, I experienced the most excruciating sciatic pain the day after I gave birth to Claire in February 2021; it exceeded even the pain of contractions when my epidural fell out for an hour right before I started pushing in labor with her.
That experience just confirmed for me that my spondylolisthesis was a consequence of having had children and just one of those things through which women have to suffer, so I… continued suffering. I had two wonderful children. What was sciatica against that?
In September 2021, I suddenly started experiencing severe pain in my right arm, radiating all the way down to my fingers. Another orthopedist - my first had since retired - sent me for xrays and then an MRI, and within six weeks I was scheduled for emergency surgery because, apparently, a disc in my c-spine was millimeters from my spinal chord and I was in danger of lasting neurological deficits. He was great and we built up enough trust over the next year of follow-up appointments that, in October 2022, I felt comfortable bringing him the file of my 2019 MRI and telling him that my sciatica might require more than just PT. He took one look at the images, sent me for updated xrays and a new MRI, and told me that surgery was a “when, not if” solution.
“Are we talking, like, sometime in the next five years?” I asked. He looked a little taken aback.
“Well, it depends on your pain tolerance, but yes. Definitely in the next five years.”
I’d always doubted my ability to assign a value to my pain - I suspect most women do - and his assurance that this was, in fact, a real medical problem confirmed that I’d probably been underestimating or, at the very least, underreporting how my body was feeling.
Until I was ready for surgery, he prescribed core-strengthening exercises either from PT or Pilates Reformer classes and told me to check in with him every six months. In spring 2023, the pain not having abated, he recommended I get cortisone shots in my spine, which blunts the pain for a lot of patients; unfortunately, I wasn’t one of them. At an appointment a few weeks after the injections, he looked at me and said, not unkindly, “Betsy, it’s time. We need to schedule this surgery.”
I had spinal fusion on August 15, 2023 - and haven’t felt a moment of sciatic pain since.
I’m thrilled, of course, but also upset. I doubt my spondylolisthesis was bad enough in 2019 to have warranted surgery and so don’t blame my original orthopedist for not having escalated treatment; according to the imaging, it definitely progressed from then to 2022. I can really only be mad at myself for not having taken my pain seriously, for not having seen doctors about it sooner, and for not having pursued real solutions. Common does not mean normal, and normal does not have to mean we have to accept it when it comes to pain - especially not pain associated with women’s reproductive systems/health/processes. (My second orthopedist says he can’t tie the spondylolisthesis to pregnancy or childbirth but the timing is notable, both the onset and that most extreme appearance of pain immediately after Claire’s birth.)
I know so many women with similar stories who, like me, have been continued to underestimate and underreport pain, particularly when it’s connected to pregnancy and childbirth. We’re getting better about destigmatizing pelvic floor issues and encouraging women to seek help for that, which is a start, but we need to keep pushing past the systemic minimizing and dismissing that so many women experience (or assume they will experience so they don’t even bother trying). I hate putting the burden of this on the victims, so here’s my plea if you feel like a survivor in any way:
Validate your friends’ pain.
Share recommendations for good doctors.
Remind them that common doesn’t necessarily mean normal and that normal doesn’t have to mean endurable.
And, whenever and wherever you can, advocate for women and our health.
Thank you.